Spina Bifida
Spina bifida is a neural tube birth defect that occurs when the spine and spinal cord don't form properly when the baby is in the womb. The neural tube forms in an embryo early in pregnancy and eventually becomes the baby's brain and spinal cord.
The neural tube should close by the 28th day after conception. In babies with spina bifida, the neural tube doesn't close all the way, so the spine which protects the spinal cord doesn’t form properly.
Spina bifida can range from mild to severe, depending on the type of spinal bifida, the size and the location of the neural tube defect, and which spinal nerves are affected.
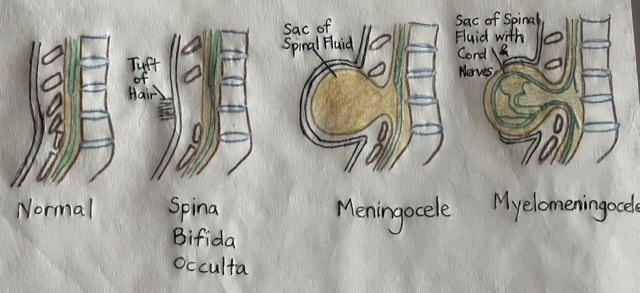
There are 3 main types of spina bifida:
- Spina Bifida Occulta: This is the most common and mildest type, and doesn’t usually cause any disability. People may not know that they have it, until a chance discovery during an unrelated xray. The spinal cord and nerves are usually fine, but there is a small gap in the spine.
- Meningocele: This is a rare type of spinal bifida, and disability ranges from having no symptoms to having issues with their bladder and bowels. In Meningocele, a sac of spinal fluid (not the spinal cord) pushes through the gap in the baby’s spine.
- Myelomeningocele: This is the most severe type of spina bifida, and baby is prone to serious infections, and may cause paralysis and bladder / bowel problems. The baby’s spine is open along one or more places in the middle or lower back. The spinal nerves (and sometimes the spinal cord also) push through the gap and the baby is born with a sac on the back, exposing the nerves, which can get damaged.
Complications:
Complications of spina bifida can range from mild to severe physical disabilities. Not all kids get all of the complications. Most spina bifida complications can be treated or managed to improve quality of life.
- Walking: How well a child with spina bifida walks will depend on the level and the size of the defect. The higher up the spine the defect is, the physical disabilities will be more severe. This is because the nerves that control the leg muscles don't work properly below the spina bifida defect. This can cause muscle weakness of the legs and occasionally paralysis.
- Musculoskeletal issues: There may be associated problems in the legs and spine because of weak muscles. Problems such as hip dislocation, bony deformities and curved spine (scoliosis) may occur.
- Skin issues: Children with spina bifida have poor sensation of their backs and legs. They cannot feel when they get a wound, and this increases the risk of the wound getting infected.
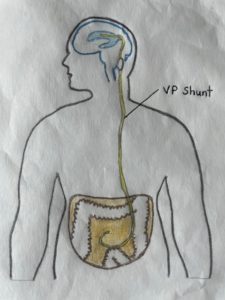
- Hydrocephalus (fluid accumulation in the brain): It is common for babies born with myelomeningocele to have accumulation of cerebrospinal fluid (CSF) in their brains. Hydrocephalus may permanently damage the brain, leading to physical and mental disabilities, and may cause death if not treated. Surgery to insert a shunt to drain the CSF is usually done, and this shunt needs to be monitored, as it may stop working or get infected.
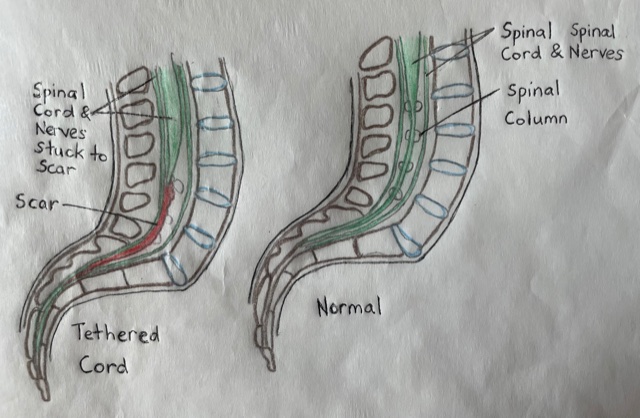
- Tethered spinal cord: The spinal cord normally moves freely inside the spinal column. For children with spina bifida, sometimes, the spinal nerves may attach to the scar from the surgery to close the defect. If the spinal nerves are stuck to the scar, it will cause abnormal stretching of the spinal nerves as the child grows. This can damage the nerves and cause loss of function of the legs, bladder or bowel.
- Bladder and bowel issues: Children with spina bifida may have problems with their bladders or bowels working properly. This is because the nerves that control the bladder and bowel are at the lowest level of the spinal cord.
How is spina bifida diagnosed?
The diagnosis is usually made with ultrasound while the baby is in the womb. Fetal ultrasound is the most accurate method to diagnose spina bifida. It can detect signs such as an open spine, or features in the brain that indicate spina bifida.
Sometimes, spina bifida is diagnosed after the birth of the baby. In this case, your doctor will request for x-rays or MRI of your baby’s spine.
Treatment:
- Surgery to close the defect – This can be done when babies are just a few days old, or even while babies are still in the womb. The surgeon will reposition the sac of spinal fluid back in place and close the opening. For babies with myelomeningocele, the surgeon will reposition the sac with the spinal nerves (and sometimes the spinal cord) back inside the baby’s body, and cover it with a layer of skin.
- Surgery to drain hydrocephalus – For babies who have accumulation of CSF in their brains, the surgeon will place a shunt (tube) in the brain with a long catheter that leads into the baby’s abdomen (VentriculoPeritoneal (VP) shunt), so that the CSF can drain into the baby’s abdomen.
- Other surgeries: As babies with spina bifida grow, other surgeries to correct the feet, hips or spine may be needed. If tethering of the spinal cord occurs, surgery may also be required to correct that.
- Bladder and bowel management: Children with spina bifida will need regular monitoring of their bladder and bowel functions, to prevent organ damage. This may include bladder function tests, kidney scans, ultrasounds, or other tests. Bladder issues: Some children may need medications, a urinary catheter or surgery to manage bladder issues. Bowel issues: Some children may require medications, suppositories or surgery to manage bowel issues.
- Equipment: Walking aids: All children with spina bifida should be able to move around independently. Depending on the severity of their physical disabilities, children with spina bifida may need braces (either AFO: Ankle Foot Orthosis, KAFO: Knee Ankle Foot Orthosis or HKAFO: Hip Knee Ankle Foot Orthosis), crutches, walkers or wheelchairs. These equipment, together with regular physiotherapy, can help children with spina bifida attain independent mobility. Other equipment: Some children may need specialised equipment such as commodes, bath chairs or other equipment to help with their activities of daily living.
- Physiotherapy: Physiotherapy is needed to strengthen muscles, improve functional abilities, and to monitor changes in musculoskeletal issues. Hydrotherapy (Aquatic Therapy), Functional Electrical Stimulation (FES), Massage may be done to complement physiotherapy exercises.
Pictures of various foot splints, elbow crutches, lightweight wheelchair.
Please feel free to reach out to us to find out more on how we can help your child.
Let's get in touch





