Seizures / Epilepsy & EEG
How the brain works?
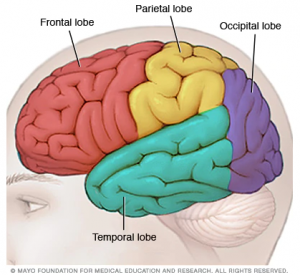
Our brain is divided into four major lobes – frontal, parietal, temporal and occipital. Different parts of the brain process different cognitive functions.
Different Lobes of the Brain
- Frontal lobe – controls how we process, organise, analyse and act on information and controls motor functions
- Parietal lobe – controls the expressive language ability and processing of body senses
- Temporal lobe – controls our memory ability and comprehension of language, organises sensory input and regulates emotions
- Occiptal lobe – deals with our visual perception and how we identify and recognise objects
Epilepsy
Epilepsy is one of the most common disorders of the nervous system. Many children with neurodevelopmental disorders suffer from seizures / epilepsy. Epilepsy is defined by recurring seizures, and is confirmed by EEG (electroencephalography - See below).
There are many different types of seizures. Anything that interrupts the normal connections between nerve cells in the brain can cause a seizure. Different seizure types often indicate different causes - brain injury is more likely to cause partial seizures, while many idiopathic epilepsy syndromes cause generalized seizures. Generalised seizures (eg: absence, atonic, tonic-clonic, myoclonic seizures) are seizures that appear to begin everywhere in the brain at once, while partial seizures (eg: simple and complex) are seizures that begin in one location of the brain. Different seizure types may be treated differently and have different prognoses. Many children have more than one type of seizure. One seizure type may progress to a different type of seizure.
Some of the more common seizures include:
- Infantile seizures: Characterised by a sudden jerk followed by stiffening. Often the arms are flung out as the knees are pulled up and the body bends forward ("jackknife seizures"). Occurs in infants before six months old. This can happen multiple times a day and can have long-term complications that affect growth and development. There is a high occurrence rate of this seizure when the child is awakening, or when he or she is trying to go to sleep.
- Absence seizures: (formerly known as petit mal): Characterised by brief episodes (lasting just a few seconds) of blank or absent stare, during which the child is not aware or responsive. Absence seizures usually occur when a child is 4 to 12 years old. Your child may have multiple absence seizures in a day. Absence seizures can happen so subtly and so quickly that you never even notice them. There is no warning before a seizure, and the child may be completely alert immediately afterward.
- Tonic-Clonic Seizures: (formerly known as grand mal): The classic form of this kind of seizure, which may not occur in every case, is characterized by distinct phases. The child goes rigid/stiff (body, arms, and legs will bend or straighten out – tonic seizure), and then convulse (shake or jerk rhythmically – clonic seizure), followed by a post-seizure period, where the child may be sleepy or tired, have problems with vision or speech, and may have a bad headache, or body aches. Not all of these phases may be seen in everyone with this type of seizure.
- Febrile Seizures: This type of seizure is provoked by a high fever and is not epilepsy, although a fever may trigger a seizure in a child who has epilepsy. They are the most common type of provoked seizures in childhood (occur in 2% to 5% of children aged 3 months to 5 years). Febrile seizures are usually tonic-clonic seizures. Febrile seizures lasting less than 15 minutes are called simple, and typically do not have long-term neurological effects. Seizures lasting more than 15 minutes are called complex and may result in long-term neurological changes in the child.
- Atonic seizures / Drop seizures: Characterised by sudden loss of muscle tone; may cause the head to drop suddenly, objects to fall from the hands, or the legs to lose strength, with falling and potential injury. During the seizure, the person is limp and unresponsive.
- Nocturnal seizures: Nocturnal seizures are usually tonic-clonic. They might occur just after a person has fallen asleep, just before waking, during daytime sleep, or while in a state of drowsiness. People who experience nocturnal seizures may find it difficult to wake up or to stay awake.
- Simple Partial Seizures: Depending on which area of the brain is involved, the child may have different symptoms. The seizure activity is limited to an isolated muscle group, such as the fingers, or to larger muscles in the arms and legs. The child is still aware of what is happening around her. Besides the motor symptoms, she may experience somatosensory (eg: sight is affected if the abnormal electrical brain function is in the part of the brain that is involved with vision), autonomic (sweating, nausea, pale), or psychic symptoms.
- Complex Partial Seizures: The person may experience an aura before the seizure occurs. The most common aura involves feelings, such as deja vu, impending doom, fear, or euphoria. Auras can also include changes in vision, hearing or sense of smell. These seizures usually start in a small area of the temporal lobe or frontal lobe of the brain. The seizures can quickly involve other areas of the brain that affect alertness and awareness, so consciousness is impaired. Losing consciousness may not mean that a person passes out. Sometimes, a person stops being aware of what's going on around him or her. When the person regains consciousness, he or she may complain of being tired or sleepy after the seizure.
- Status Epilepticus: Status epilepticus occurs when a seizure continues for a long time (more than half an hour), or when a child has several seizures without time to recover between them. It can happen with any seizure type.
NB: Not all jerks / sudden movements of your child are symptoms of seizures. Please consult your doctor / paediatrician for an accurate diagnosis.
How are Seizures / Epilepsy diagnosed?
If you suspect that your child has epilepsy, it is important to get the correct diagnosis as soon as possible, so that the appropriate treatment can be given. The doctor will have to rule out medical conditions that may cause seizures, by going through the medical history, performing a neurological examination, sending your child for blood tests, and scheduling an EEG.
What is EEG?
Electroencephalography (EEG) detects and records abnormalities in your brain waves, or in the spontaneous electrical activity of your brain over a period of time. This is the most common test to diagnose epilepsy.
How it is measured?
A few electrodes or sensors are strategically placed on the scalp to measure tiny electrical charges that result from the activity of your brain cells.
Who needs it?
Children with suspected seizures to confirm the diagnosis of epilepsy. When epilepsy is present, seizure activity will appear as rapid spiking waves on the EEG. The test can also be used to diagnose other disorders that influence brain activity, evaluate trauma, the extent of brain damage, or may be used to monitor blood flow in the brain during surgical procedures.
What is the process like?
An EEG may be done as an outpatient, or as part of thew child’s stay in a hospital where the child may be required to sleep through the procedure. Your child may be given a sedative to help your child to relax and/or sleep before the test begins. The technician may put sticky gel adhesive on about 20 electrodes, which will then be attached to various spots on your child’s scalp, or a cap containing the electrodes will be used. The recording begins while your child is at rest, and your child may be tested with various stimuli to produce brain wave activity that does not show up while at rest, eg: exposed to bright, flashing light. After the test is completed, the electrodes will be removed and the glue will be washed off with warm water or acetone. If your child was given a sedative, he/she may be drowsy for a few hours.
How long is one session?
Depending on the doctor and the seizure activity that your child displays, it might take just 1 hour. Or the doctor may decide to monitor the brain’s electrical activity for up to 24 hours.
What are the risks of an EEG?
The EEG is a safe procedure that has been used for many years. It causes no discomfort and does not produce any sensation. Skin irritation or redness may be present at the locations where the electrodes were placed, but this will wear off in a few hours. When someone has epilepsy or a seizure disorder, there is a very small risk that the stimuli presented during the test (such as a flashing light) may cause a seizure. However, the technician performing the EEG is trained to safely manage the situation should this occur.
What do the EEG results mean?
You won't normally get your results on the same day. A neurologist (someone who specializes in nervous system disorders) will analyse the EEG recordings and will then send the results to the doctor who requested the test. Your doctor may schedule an appointment to go over the test results with you.
Common Treatment Options for Seizures / Epilepsy:
Treatment options include anti-epileptic drugs, ketogenic diet or brain surgery for severe cases.
Ketogenic Diet:
The ketogenic diet is a high-fat, low-carbohydrate diet, where the body burns fat instead of carbohydrates for energy. For children on multiple anti-epileptic medication, the ketogenic diet has been used and found to be effective for children with epilepsy. If you are interested in the ketogenic diet for your child, please speak to your child's paediatrician before starting the ketogenic diet. Children on the ketogenic diet need to be followed up regularly by a dietitian experienced in the ketogenic diet for children with epilepsy. The dietitian will have to adjust the diet based on each child's needs, so that normal growth and weight gain can occur.
Please follow this link for the article that describes how the ketogenic diet works in epilepsy, and the benefits and side effects of this diet.