Chest Physiotherapy for Children
By Dr Janell Lee, DPT, NZRP, SRP, C/NDT (paeds), CIMI
Specialist paediatric physiotherapist
Chest physiotherapy (CPT), or respiratory physiotherapy, with postural drainage is the standard treatment for mobilising airway secretions in many types of respiratory dysfunction / disorders.
Your child might be referred for chest physiotherapy if he / she has secretion retention, collapsed lung, shallow or fast rate of breathing, unable to maintain oxygenation, post-surgery, etc. Chest physiotherapy is more than just a physiotherapist ‘thumping’ your child’s chest when he/she has a lung infection. The range of what chest physiotherapy constitutes is too wide to cover in an article, so this will be a general write-up on the more common chest physiotherapy techniques used.
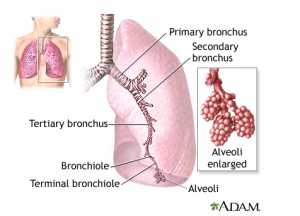
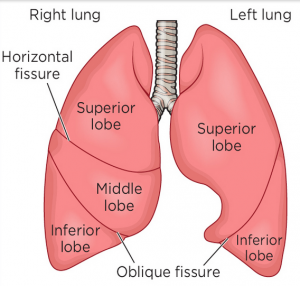
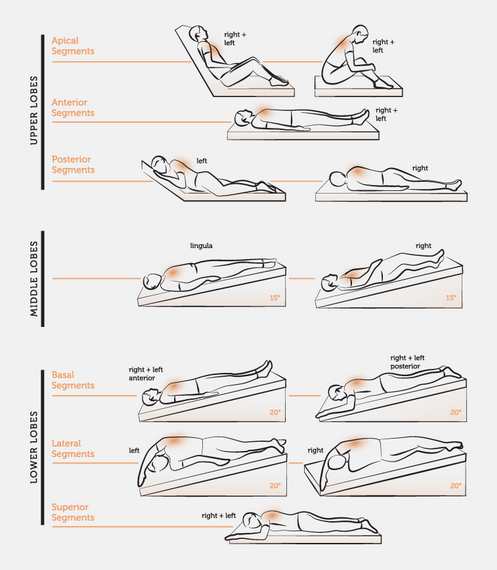
The lungs are divided into right and left lungs and each lung is made up of different lobes or segments. Depending on which lobe(s) the secretion is retained in, the physiotherapist will position your child in the position(s) required to drain the lungs. The positions may differ from child to child as certain conditions (eg: increased intracranial pressure, reflux, etc.) make it dangerous for the classic postural drainage positions to be used and may need to be modified. So please consult with your physiotherapist before you start any postural drainage positions.
Postural Drainage Positions
‘Thumping’ or percussion as it is called is just one manual technique that physiotherapists use to loosen up secretions that are in your child’s lungs. Other techniques that the physiotherapist may use to loosen up secretions in the lungs include vibration and shaking. Your child may be taught to huff or cough effectively to expectorate the secretions after the secretions have been loosened up from the lungs. If your child is unable to huff or cough, the airway secretions may be removed using a suction catether via the nose, mouth and/or tracheostomy (hole in throat leading directly to airway). Your child may be given a tracheostomy if your child has copious amounts of secretions that need frequent suctioning, if more long-term ventilation is required or if your child’s airways are ‘floppy’ and need more support.
Sometimes, your child may be able to cough, but the coughs are not strong enough to expectorate the secretions. The physiotherapist may teach your child the use of a “cough assist” machine at the hospitals to facilitate your child to have a stronger cough, in the hope that your child will be able to cough out the secretions without needing to be suctioned.
There are devices of respiratory physiotherapy which offer greater independence to the child with chronic lung disease. Examples of these devices include the Acapella, Flutter, Thera-PEP, etc. These devices facilitate and improve mobilisation of mucus from airways, so that improved lung function can be achieved. These devices are safe and can be used as an alternative airway clearance to conventional CPT. Your physiotherapist will need to teach your child how to use them correctly, so that they will be effective.
There are certain respiratory conditions where copious amounts of thick, sticky secretions are produced daily by the lungs (eg: cystic fibrosis, bronchiectasis etc), where the lifespan of your child is dependent on the removal of such secretions from the lungs, so that it doesn’t become a chest infection. Rigorous chest physiotherapy has to be incorporated into the care of your child from young, so that chest physiotherapy becomes routine. We may start with postural drainage and manual techniques when your child is very young. We may teach lots of blowing games such as bubbles, balloons, windmills, whistles, etc. to encourage bigger breaths and will advise the child to be active in general. As the child grows older, we may progress to teaching him the use of a respiratory devices to encourage more independence in chest physiotherapy and encouraging a life-long engagement in exercises and sports.
Sometimes, your child may be unable to maintain oxygen saturation which may not be due to secretion retention, but may be due to the inability to take sufficiently deep breaths. This could be due different reasons such as neuromuscular disorders, muscular dystrophies, pain, fatigue etc. Your child’s doctor may prescribed oxygen for your child during the day or at night, either through nasal prongs, face mask, CPAP or BIPAP machines.
In such cases, the physiotherapist may prescribe an incentive spirometer for your child to teach him / her how to take deeper breaths in. Your child is taught how to suck air in through the mouth and watch the number of balls (or a circular disc) rising and staying up.

For people with weak respiratory muscles, 'The Breather' is an evidenced-based Inspiratory/Expiratory Respiratory Muscle Training (RMT) device. It trains both inspiratory and expiratory muscles independently. This helps to promote diaphragmatic breathing, reduce shortness of breath, improve respiratory support for safe swallow function and improve protective cough.
The physiotherapist may teach your child certain positions to adopt for more effective breathing, breath control techniques so that your child doesn’t tire as quickly, teach slow, deep breathing via abdominals versus fast, shallow chest breathing.
Disclaimer: This article is not meant for anyone to self-diagnose or to self-treat without consulting your physiotherapist. Please note that not all treatment techniques described here are suitable for all kids.
Please feel free to reach out to us to learn how to improve your child's respiratory status, either through postural drainage positions, chest clearance techniques or inspiratory / expiratory muscle training.
Let's get in touch